
Resources, protocols, workflow, & tip sheets for providers & clinic teams
We are developing resources to assist with the implementation of the Disability and Accommodations Tab. This section will be updated as these resources are developed.
Cognitive impairment can be caused by Alzheimer’s disease and other dementias in addition to conditions such as stroke, traumatic brain injury, and developmental disabilities. Patients with cognitive impairment may struggle to remember, learn new things, concentrate, or make decisions that affect their everyday life.
A few commons symptoms of cognitive impairment include the following:
- Memory loss
- Frequently asking the same question or repeating the same story over and over
- Not recognizing familiar people and places
- Having trouble exercising judgment, such as knowing what to do in an emergency
- Changes in mood or behavior
- Vision problems
- Difficulty planning and carrying out tasks
| Address the patient directly, even if his or her cognitive capacity is diminished | |
| Gain the patient's attention by sitting at the same eye level as the patient and maintain eye contact. | |
| Speak at a normal volume and resist the temptation to speak loudly | |
| Orient the patient by explaining (or re-explaining) who you are and what you will be doing | |
To help patients understand better:
| |
| Remember that many older patients may have hearing or vision problems which can add to their confusion. | |
| Eliminate distractions and minimize background noises, if possible, by rooming the patient early. | |
| Leverage the support person or guardian and offer a checklist of next steps and resources. | |
| Address potential issues of driving, getting lost, and home safety with the patient. | |
| Call the patient to follow up on instructions after outpatient visits. |
Please see Michigan Medicine’s Visitor Guidelines During COVID-19, including the Guidelines for Supporting Adult Patients with Disabilities During the COVID-19 Public Health Emergency. Questions regarding policy modifications should be referred to Patient Relations and Clinical Risk at 734-936-4330.
Michigan Medicine’s internal resources webpage on Cognitive Disorders contains American Academy of Neurology Position Papers, Clinical Tools and Algorithms, and Classics Publications.
Cognitive Disorders Clinic
Consider referring the patient to the Cognitive Disorders Clinic if the patient has not been seen by a specialist yet. To schedule an appointment at the Cognitive Disorders Clinic, call 734-764-6831.
Michigan Adapted Cognitive Assessment Clinic (MACAC)
Consider referring pediatric patients with unique testing needs due to severe motor and/or speech-language difficulties to the Michigan Adapted Cognitive Assessment Clinic (MACAC).
Michigan Alzheimer’s Disease Center (MADC)
The Michigan Alzheimer’s Disease Center has a dedicated resource page containing additional disease information, local and national resources, book recommendations, and virtual exercise programs.
This self-paced certificate is designed for healthcare professionals who deliver or plan to deliver person- and family-centered care to people living with memory loss or dementia, including social workers; nurses; primary care physicians; physical therapists; occupational therapists; health educators; and administrators. Participants will gain clinical knowledge and skills in culturally competent assessment, care planning, and state-of-the-art clinical intervention. Learn more about the program here.

| Ask the patient for the best way to achieve effective communication. Some may require sign language. For others, it simply may be lipreading. |

| Look directly at the patient. Avoid looking towards the interpreter. Avoid having a window or light behind you as those make it harder to read lips. |
Speak clearly and slowly
| |

| Consider using a medical scribe to reduce the need to type into a medical record while engaging the patient. |

| DHH patients are no more or less intelligent and capable than hearing patients. Avoid talking down or dumbing down the topic. |

| Ask about patients’ views on their hearing loss. For some, hearing loss may be a form of a cultural identity instead of a disability. |
Call 734-936-7021 or email [email protected] to arrange for an ASL interpreter upon appointment scheduling as soon as possible.
Communication Access Realtime Translation (CART)
Communication Access Realtime Translation (CART) or real-time captioning is the instant translation of spoken English into text using a stenotype machine, notebook computer and software. The text can be displayed on an individual's computer monitor or tablet, projected onto a screen, or combined with a video presentation as captions. This helps people with hearing loss access information in a wide variety of settings.
To arrange for CART service, page 31019 or email [email protected] upon appointment scheduling as soon as possible.
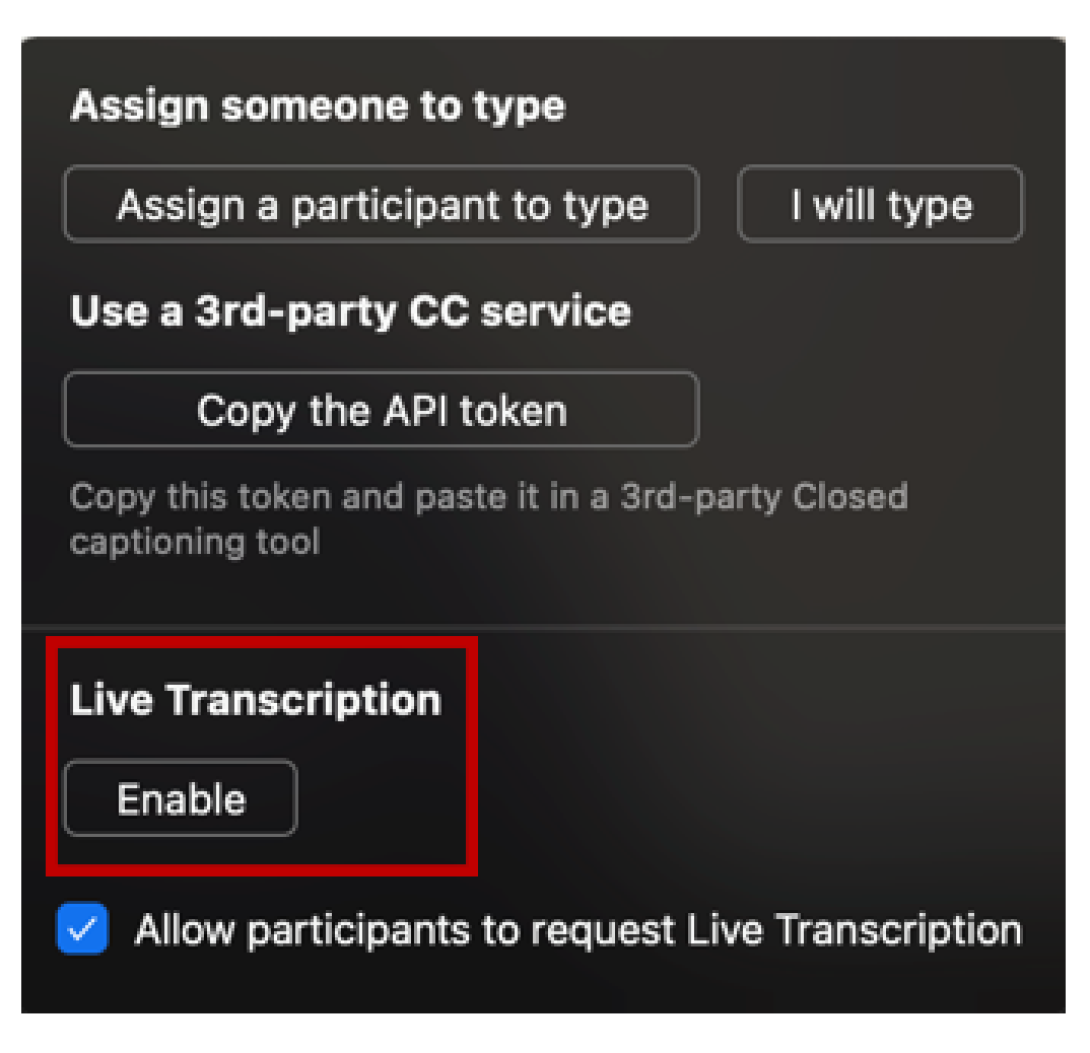
Zoom Video Visit CC/Live Captioning
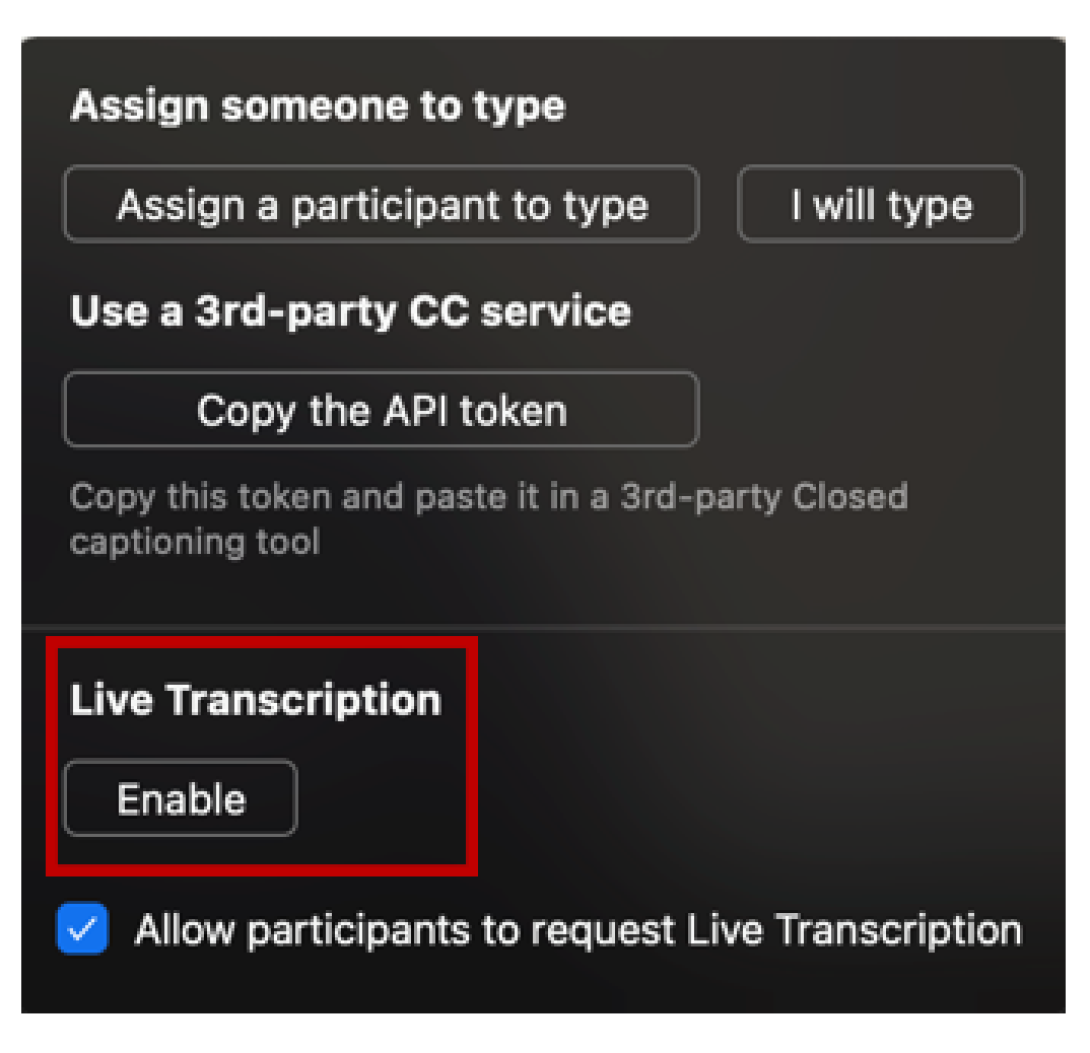
Live captioning is an auto transcribe feature available on Zoom video and can be used during virtual visits with patients. The text can be displayed once this feature can be enabled at the bottom of the screen. To enable CC/Live Captioning during virtual visits with patients, follow the steps below:
Step 1: See bottom bar for Live Transcript button. Select this.

Step 2: Select enable under Live Transcription. This will activate the live transcription feature.
Educational, instructional or any critical information should be written or given in print form in advance of discussion whenever possible. When sharing any patient education videos, check that the correct version of the video with the subtitles enabled is shared with the patient.
Ask patient what type of device they use/need and how best to work with them. Pocket talkers are available upon request - email [email protected] or page 31019
Pocket talker - A Pocketalker is a personal amplifier. It is a headset with an amplifying system. It looks like what a Walkman ® used to look like; a little box with a microphone on it wired to a headset. It provides some amplification for sound. It can be useful particularly in an in-patient setting where you need some amplification, and there may not be an opportunity for the person to go to an audiologist to be fitted with hearing aids. This is a solution for "in the moment."
Minimize any environmental noise that might effect communication (e.g., fans, alarms, hallway noises).

Clear masks can be ordered from supply chain 82295. FDA approved clear masks currently include:
- Consider utilizing whiteboards
- Laminated cards with written instructions can be helpful during the check-in process
Intellectual disability is used to define a developmental disorder characterized by impaired social functioning and limited cognitive ability that have developed before the age of 18 years. Patients with IDD may have difficulties with abstract concepts and the subtleties of interpersonal interactions. The kind of support needed may vary depending on each patient’s cognitive ability and the presence of other associated developmental disabilities such as cerebral palsy, autism or sensory impairments.
- Someone with a mild intellectual disability (IQ 50-70) might be able to read and write. Some may not have learned to read or write, so sensitivity is required when requesting patients to read information or complete written forms.
- Someone with a moderate intellectual disability (IQ 35-50) can learn to recognize some words in context. With adequate vision, these patients will benefit from visual prompts to clarify meaning.
- Someone with a severe (IQ 20-35) or profound (IQ <20) intellectual disability likely has little or no speech. These patients will rely on facial expression, body language, and gestures to express their needs. Using objects can be helpful to facilitate understanding.
| Make sure you have the patient’s attention by addressing the patient by name, making an eye contact and/or using touch. | |

| Follow your clinic process to lengthen the appointment time. |

| When unsure of the patient’s ability to understand, assume competence not a lack of understanding. Adjust your method of communication based on patients’ response. |

| Use simple, concrete language in short sentences without idioms, irony, or metaphors. Give direct requests. |
| Use an appropriate tone of voice that is consistent with the patient’s age. Treat an adult patient with IDD as an adult. | |

| Don’t rush. Allow time for patient to listen and process what you say. |
| Leverage the support person or guardian for behavior management, communication, and patient preferences. | |
| Eliminate distractions and minimize background noises if possible by rooming the patient early. | |

| Use dimmable light switches to minimize the sensory input for patients with sensory integration issues. |
| Avoid sensory overload by providing information gradually and clearly. | |
| Assign an accessible examination room to accommodate wheelchairs and other adaptive equipment. | |
If the patient doesn’t understand:
If you don’t understand:
|
Please see Michigan Medicine’s Visitor Guidelines During COVID-19, including the Guidelines for Supporting Adult Patients with Disabilities During the COVID-19 Public Health Emergency. Questions regarding policy modifications should be referred to Patient Relations and Clinical Risk at 734-936-4330.
To learn more about Michigan Medicine’s policy on service animals, please watch this video. It has been designed to provide real life examples on how to handle patients with service animals and describes the rights of patients with service animals. You may also download a FAQ sheet to share with colleagues.
Have toys or distracting objects (e.g., anything with sensory properties) available and/or ask families about topics that are especially engaging to the patient.
Visual supports can establish predictability, reduce anxiety, and promote more effective coping during a medical visit. A First-Then Board or a visual schedule can be adopted to communicate with the patient better.
- A First-Then Board can motivate patients to engage in medical procedures by clarifying that the preferred items or activities will be available after it is over.
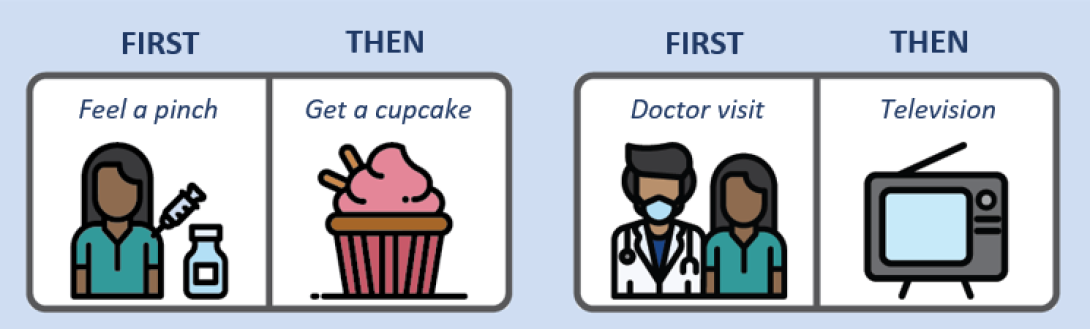
- A Visual Schedule maps out activities that will happen during a visit. When designing the schedule, try to mix in preferred activities with non-preferred ones and finish with a positive activity. When each task is completed, work with the patient to check the schedule before transitioning to the next activity. Provide praise and/or other reinforcement to the patient for following the schedule.


| Introduce yourself by sharing your name and role. |

| Orient the patient to the room, ensuring that the patient is aware of any obstacles and can locate the emergency call bell. |

| Speak directly to the patient using a normal tone of voice. Avoid shouting. |

| Be specific and descriptive. Avoid using the words “here” and “there." |
| Be cognizant that some patients may suffer from light sensitivity. Check with the patient on their preferences for lights and blinds. | |

| Always ask what the patient would like or need; don’t assume. |
Any patient education videos should have the audio descriptors turned on. When sharing any patient education videos, check that the correct link with the enabled audio descriptors is shared with the patient. If text or an image appears on the screen, it needs to be read aloud or described.
For patients with a refreshable braille reader, digital format braille can be produced in a couple of different formats. Please contact Jane Berliss-Vincent at [email protected] or Knox Center staff at [email protected] or call (734) 936-3794 to arrange for this service.
Dimmer switches may alleviate eye strain for the patient. We recommend that your clinic/floor identifies rooms with dimmable switches prior to rooming the patients. If dimmers are not available, consider a room with a window and adjust the blinds.
In a room without a dimmer light, check with the patient if they prefer the overhead lights off. Clip-on lights with dimmable and hue switches can also be utilized instead of the overhead lights. We are currently building the Disability Cart that includes clip-on lights. This page will be updated with more information on how request one.
A large-font AVS is now available under the Snapshot reports. Search “AMB AVS – large font” in the search bar on the top left. This will increase the font size for the report along with the After Visit Summary sheets for the patients.
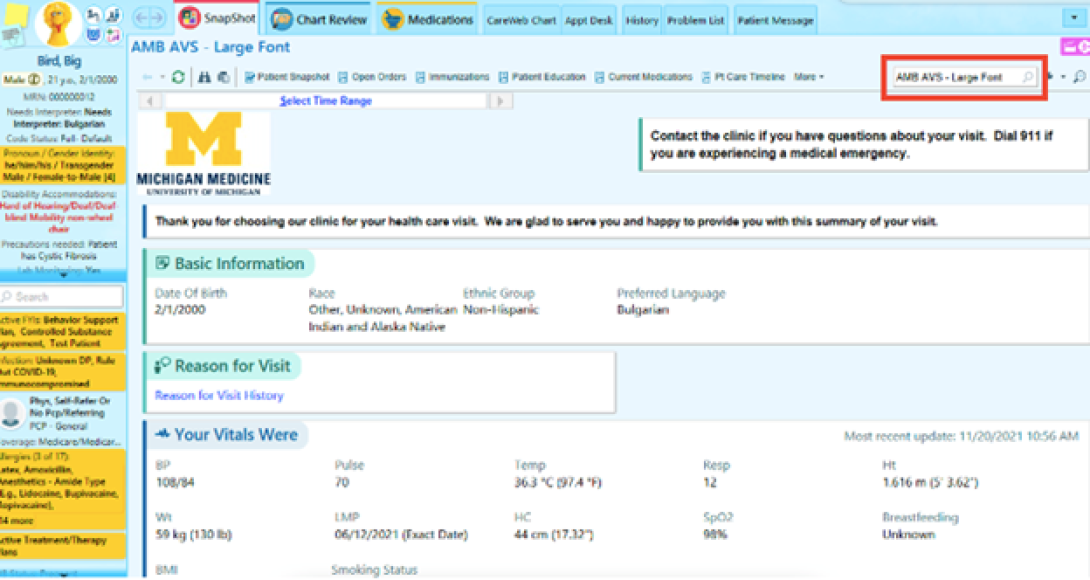
Consider using a highlight to emphasize the important sections in the AVS.
General Diet: Large print and pictorial menus are available in PFANS internal website. Patients can also request a large print or picture menu by calling the meal order line (3-8080).
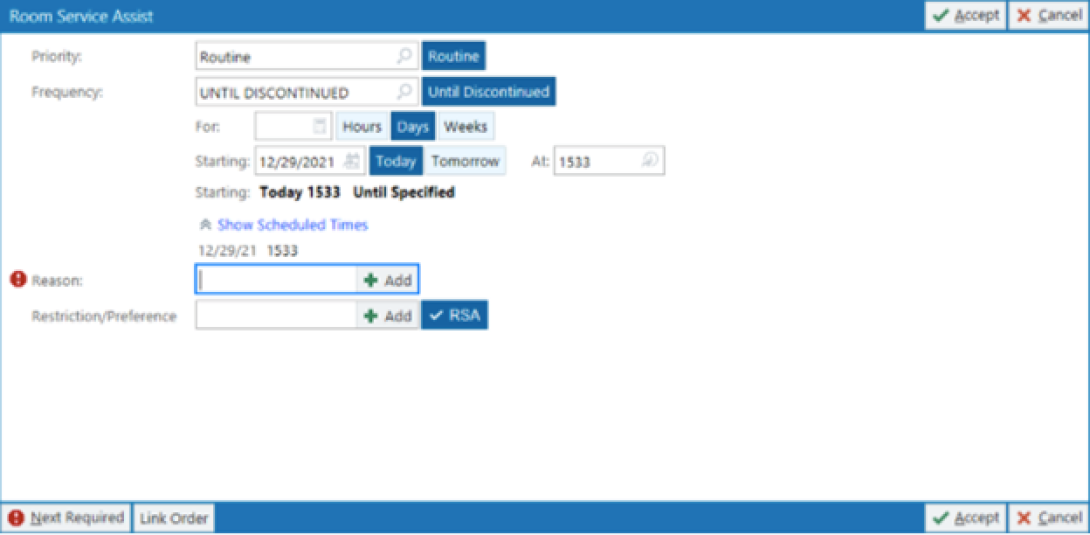
Therapeutic Diet: Therapeutic menu is currently not available in large-print. For patient who needs assistance with diet restrictions, the call center staff will assist with meal selections when they call to order. Medical staff can order “Room Service Assistant” for low vision/blind patients, and the call center staff will visit the patient at the bedside to assist with meal ordering.
Screen readers are software programs that allow blind or visually impaired users to hear/magnify the text that is displayed on the computer screen. Patients may also use this technology to fill out forms.
In partnership with Michigan Medicine’s Office of Patient Experience and multiple community organizations, CDHW has developed a training to help Michigan Medicine affiliates serve as human guides to patients who are blind.
To learn more about Michigan Medicine’s policy on service animals, please watch this video. It has been designed to provide real life examples on how to handle patients with service animals and describes the rights of patients with service animals. You may also download a FAQ sheet to share with colleagues.
Call Light/TV Controller Adaptation

Standard call lights can be adapted by using protective bump dots. We are currently in the process of building ADA Cart Kit, which will include protective dots. In the interim, protective dots like the one shown in the picture can be used. We are currently in the process of building ADA Cart Kit, which will include protective dots. In the interim, protective dots like the one shown in the picture can be used.
Follow the steps below to make the call light more accessible:
- Place the clear dot over the nursing symbol and the light symbol. Using the clear dot ensures that the symbols are visible to patient attendants.

- Place the green felt dots over the TV on/off buttons and on the side under the volume up/down wheel.
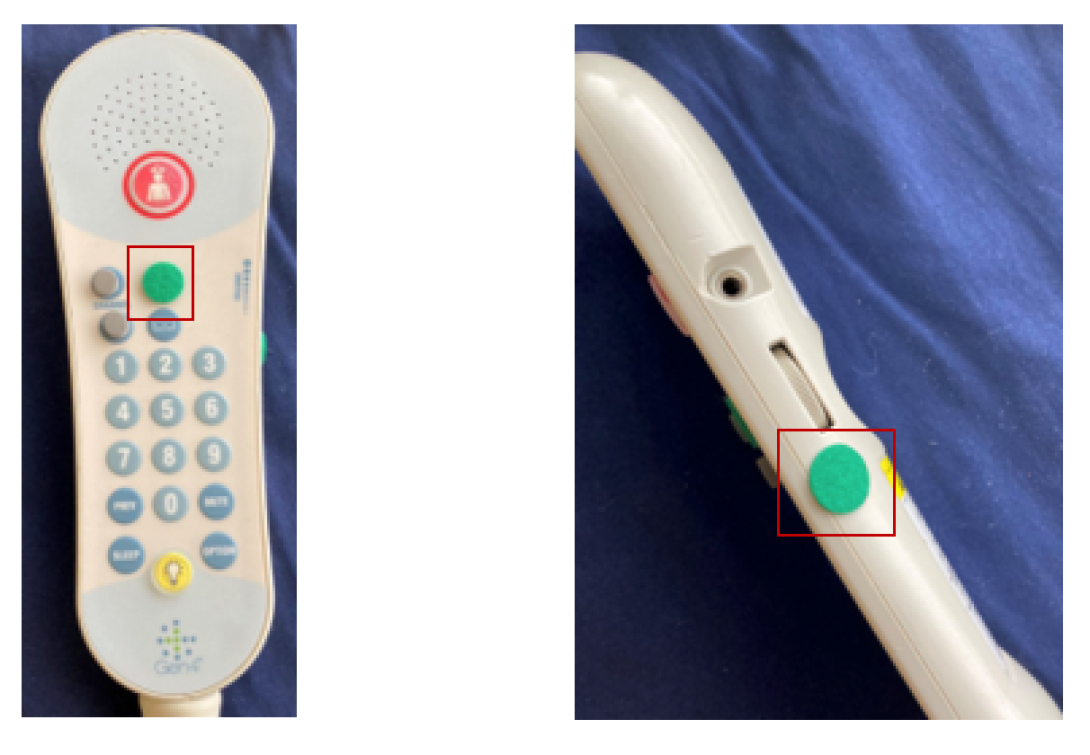
- Place the grey felt dots over the channel buttons.
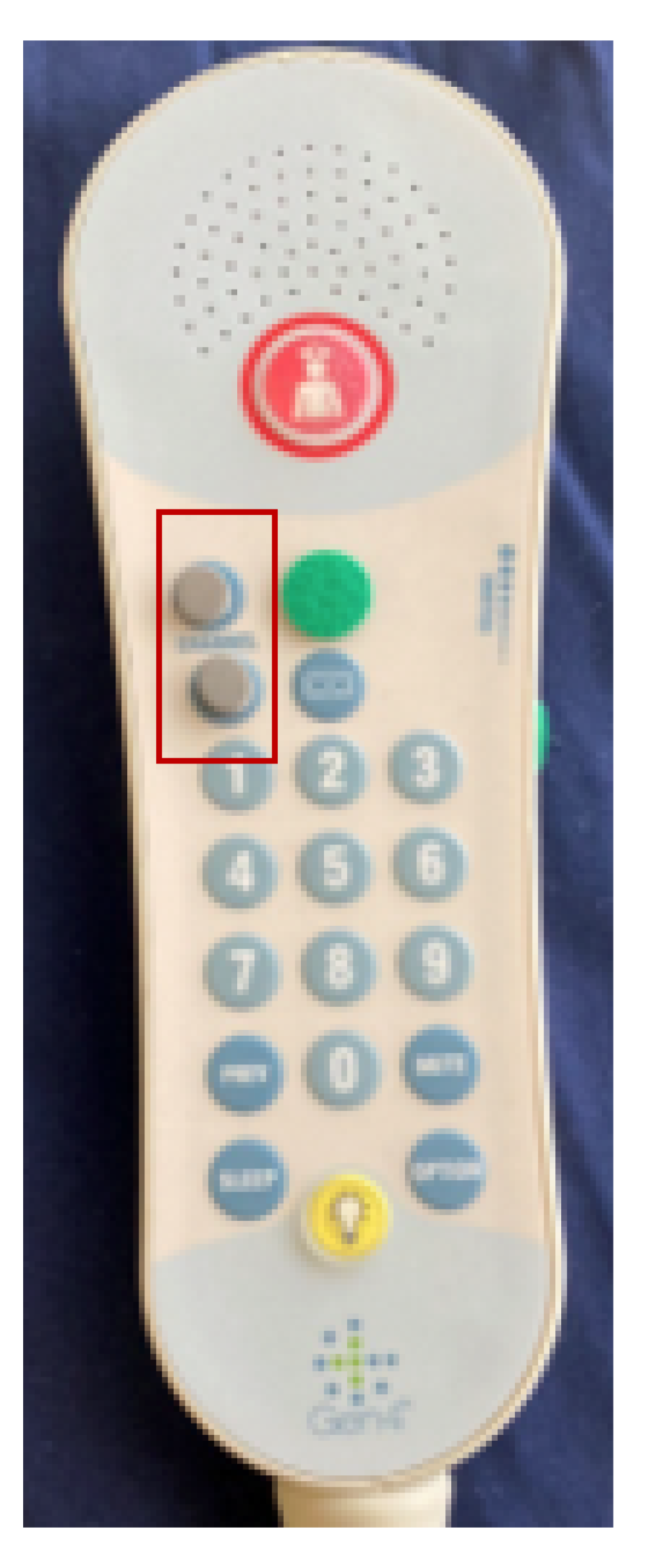
When orienting the patient to the patient controller, compare it to a shoe: “The cord is attached to the heel, which is where the light switch is located. At about where the shoelaces are placed is where the TV on/off buttons can be found. To the left of the TV button is the channel buttons. The nurse call light is located past the shoestring area in the middle of the toe area. It has the biggest dot. Volume controls is on the side and has the same dot as the TV.” Combine this with hand-over-hand tactile learning and have the patient teach locations back to demonstrate recall.
The bump dots can be scraped off by using detachol. Alternatively, floors can also keep the adapted call lights with the bump dots on the side and swap it out whenever the need arises.
Adults, Young Adults and Adolescent Patients with mental health concerns might display:
- Prolonged depression (sadness or irritability) or suicidal thoughts
- Feelings of extreme highs and lows
- Excessive fears, worries and anxieties
- Social withdrawal
- Dramatic changes in eating or sleeping habits
- Strong displays of anger
- Delusions or hallucinations
- Growing inability to cope with daily problems and activities
- Numerous unexplained physical ailments
- Substance abuse
| Make sure you have the patient’s attention by addressing the patient by name, making an eye contact and/or using touch. | |

| Use simple, concrete language in short sentences without idioms, irony, or metaphors. Give direct requests. |

| Don’t rush. Allow time for patient to listen and process what you say. |
| Leverage the support person or guardian for behavior management, communication, and patient preferences. | |
If the patient doesn’t understand:
If you don’t understand:
| |
| Eliminate distractions and minimize background noises, if possible, by rooming the patient early. | |
| Avoid sensory overload by providing information gradually and clearly. | |
| Treat adults as adults. Do not patronize, condescend, or threaten when communicating with the person. | |
| Do not make decisions for the person or assume that you know the person's preferences. |
Please see Michigan Medicine’s Visitor Guidelines During COVID-19, including the Guidelines for Supporting Adult Patients with Disabilities During the COVID-19 Public Health Emergency (PDF). Questions regarding policy modifications should be referred to Patient Relations and Clinical Risk at 734-936-4330.
To learn more about Michigan Medicine’s policy on service animals, please watch this video. It has been designed to provide real life examples on how to handle patients with service animals and describes the rights of patients with service animals. You may also download a FAQ sheet to share with colleagues.
Also known as a psychiatric advance directive (PAD), the advance directives for mental health care legally documents the patient’s preferences for future mental health treatment and allows for the appointment of a proxy to interpret those preferences during a mental health crisis.
- Path Projects: The PATH (Projects for Assistance in Transition from Homelessness) provides funds for services to persons with mental illness, including those with substance use disorders who are experiencing homelessness or at risk of becoming homeless.
- Shelter Plus Care: The Shelter Plus Care Program (S+C) links rental assistance for homeless individuals with disabilities and their families.
People with mobility disabilities are not all the same - they use mobility devices of different types, sizes, and weight, transfer in different ways, and have varying levels of physical ability. If you are unsure, it is encouraged to ask questions. Understanding what assistance, if any, is needed and how to provide it, ensures safe and accessible health care for people with mobility disabilities.

| Clear a path of access to the room. |

| Respect personal space, including wheelchair and assistive devices. |

| Do not examine patients while seated in their wheelchairs if the examination requires a person to lie down. |

| Do not lean against or hang on the patient’s wheelchair. Keep in mind that people with disabilities treat their chairs as extensions of their bodies. |

| Place yourself at eye level when speaking with someone in a wheelchair. |

| Room the patient in a room with an adjustable exam table. If an adjustable exam table is not available, room the patient in the largest room. |
Wheelchair users and patients with other activity limitations have difficulty may have difficulty getting onto a fixed-height examination table that is typically 32 inches tall. Adjustable height examination tables capable of achieving a low height in the range of 18 inches can remove barriers to access.
In the absence of adjustable exam tables, a therapy table may be used. Wheelchair users and patients with other activity limitations should be lifted or assisted onto the exam table.
Below are some videos on how to use various transfer equipment such as a Hoyer Lift and a transfer board.
Transfers Intro
Here is a quick video on some transfer techniques and steps to remember:
- Make sure that the patient is comfortable before transferring the patient
- Keep straight back in a neutral position and stay low with knees slightly bent
- Stay close to the patient when assisting the patients
Transfer Options
Hoyer Lift Transfer
It is recommended that you watch this video prior to operating a Hoyer Lift even if you had a training before. When operating a Hoyer Lift, please remember to:
- Check that the sling is appropriately sized – the harness should be large enough to wrap around the patient’s torso, but not too large that the patient will slip through
- Check that the brakes are locked
- Check that the bottom crease of the harness is all the way down to the bottom of the patient’s buttocks
- When cross the two-leg straps, ensure that the patient’s bottom does not fall behind in the whole harness
- When lacing the loop in the ring of the Hoyer, ensure that the cross position of the loop is maintained
- Undo any straps or belts the patient may have attached to the wheelchair
- Hold the boom, which is the long-angled bar at the top, while moving the patient to minimize the swing
Transfers Popover
Transfer Popover is used by patients who have good upper body strength but are not able to use their legs. Here is a video on some transfer popover techniques and steps to remember:
- Have the patient lean forward to help put on the gait belt
- Make sure the brakes are on
- The patient will turn their hips and will use upper extremities to push through the arms and pop hips over to the surface
- Stay in front of the patient in case the patient loses balance or needs help
In case the patient cannot perform popover transfers safely, use a sliding board:
- Tuck the board underneath the patient’s thigh
- Have the board at an angle with the endpoint on the surface
- Stay in front of the patient while the patient scoots over to the surface
- Make sure that the patient’s feet have moved along with the body
- Once the patient is balanced, remove the board
- Do not bend at your back when assisting the patient, use your knees
Transfers Sliding Board
Here is a video on how to operate transfers sliding board and some steps to remember:
- Pull the brake on the patient’s chair
- Have the patient lean forward to place the gait belt
- The patient will twist in the chair and place the board under their thigh
- Keep a hand on the patient’s shoulder and hold on to the patient’s leg
- Make sure that the patient is balanced before removing the board or adjusting the patient’s legs onto the table
- When moving the patient back to the chair, have the chair at a slight angle to the patient
- Lift the patient’s leg and place one foot on the pedal
- Ensure that both brakes are on
- Place one end of the board under the patient’s thigh and the other end on the chair
- Stay close to the patient with one hand over the patient’s shoulder and the other hand on the patient’s leg. The patient will scoot over to the chair
- Take the gait belt off
Use the largest patient room with an adjustable exam table and remove extra chairs in the room.
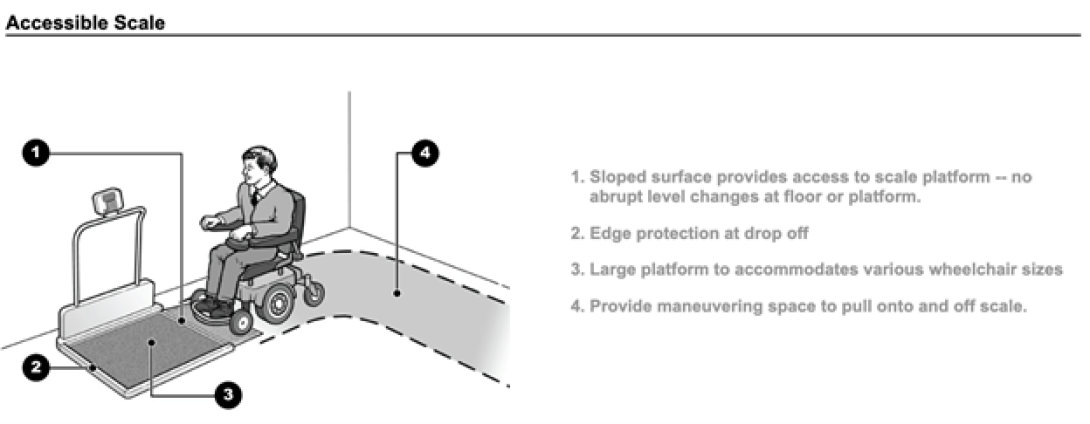
A wheelchair-accessible scale should have a sloped platform large enough to fit a wheelchair with a high weight capacity to weigh a patient while he or she is seated in the wheelchair. There should be enough maneuvering space to pull onto and off the scale.
Please see Michigan Medicine’s Visitor Guidelines During COVID-19, including the Guidelines for Supporting Adult Patients with Disabilities During the COVID-19 Public Health Emergency (PDF). Questions regarding policy modifications should be referred to Patient Relations and Clinical Risk at 734-936-4330.
Patients with speech and or communication disorders may have difficulty with articulating words, voice strength, or participating in verbal and nonverbal communication. The symptoms can range from a slight stutter to the inability to use speech or language to communicate.

| Familiarize with how the patient communicates before medical interview. Find out whether the patient already has a reliable and preferred communication method. |

| Reduce Rate: Slow down! Pause between phrases, one idea at a time, allow more time for patient to respond. |

| Assist with communication. Ask questions in a different way to help patient understand (e.g., multiple choice; yes/no). |

| Mix communication method. Keep a small whiteboard/pad of paper handy to write key words or draw. Use pictures, alphabet boards, and gestures. |

| Engage the patient first. Communicate directly with the patient. Do not ignore patient and talk only to family/caregiver. |
Note. Adapted from “Medical education: Preparing professionals to enhance communication access in healthcare settings,” by K. Yorkston, C. Baylor, M. Burns, M. Morris, & T. McNalley, in S. Blackstone, D. Beukelman, & K. Yorkston (Eds.), Patient-Provider Communication: Roles for Speech-Language Pathologists and Other Health Care Professionals (p. 55), 2015, San Diego, CA: Plural Publishing, Inc. Copyright 2015 by Plural Publishing, Inc.
Live captioning is an auto transcribe feature available on Zoom video and can be used during virtual visits with patients. The text can be displayed once this feature can be enabled at the bottom of the screen. To enable CC/Live Captioning during virtual visits with patients, follow the steps below:
Step 1: See bottom bar for Live Transcript button. Select this.

Step 2: Select enable under Live Transcription. This will activate the live transcription feature.
We are also currently building the Disability Cart that includes whiteboards. This page will be updated with more information on how request one. It is recommended that your clinic or floor acquire a few whiteboards to use for immediate use.
Minimize any environmental noise that might effect communication (e.g., fans, alarms, hallway noises).
Please see Michigan Medicine’s Visitor Guidelines During COVID-19, including the Guidelines for Supporting Adult Patients with Disabilities During the COVID-19 Public Health Emergency (PDF). Questions regarding policy modifications should be referred to Patient Relations and Clinical Risk at 734-936-4330.
For any questions or concerns around the patient rights, please reach out to the Patient Civil Rights Coordinator at [email protected]. For additional guidance and support for identifying resources on topics such as accommodations, physical accessibility, service animals and disability inclusion and awareness, you can also reach out to the ADA team at [email protected].
Lower Level Suite 6,
Ann Arbor, Michigan 48108